- Research focus
- How to conduct research on Fora Health in line with patient perspectives
- Participant focus
- People living with bipolar disorder and depression
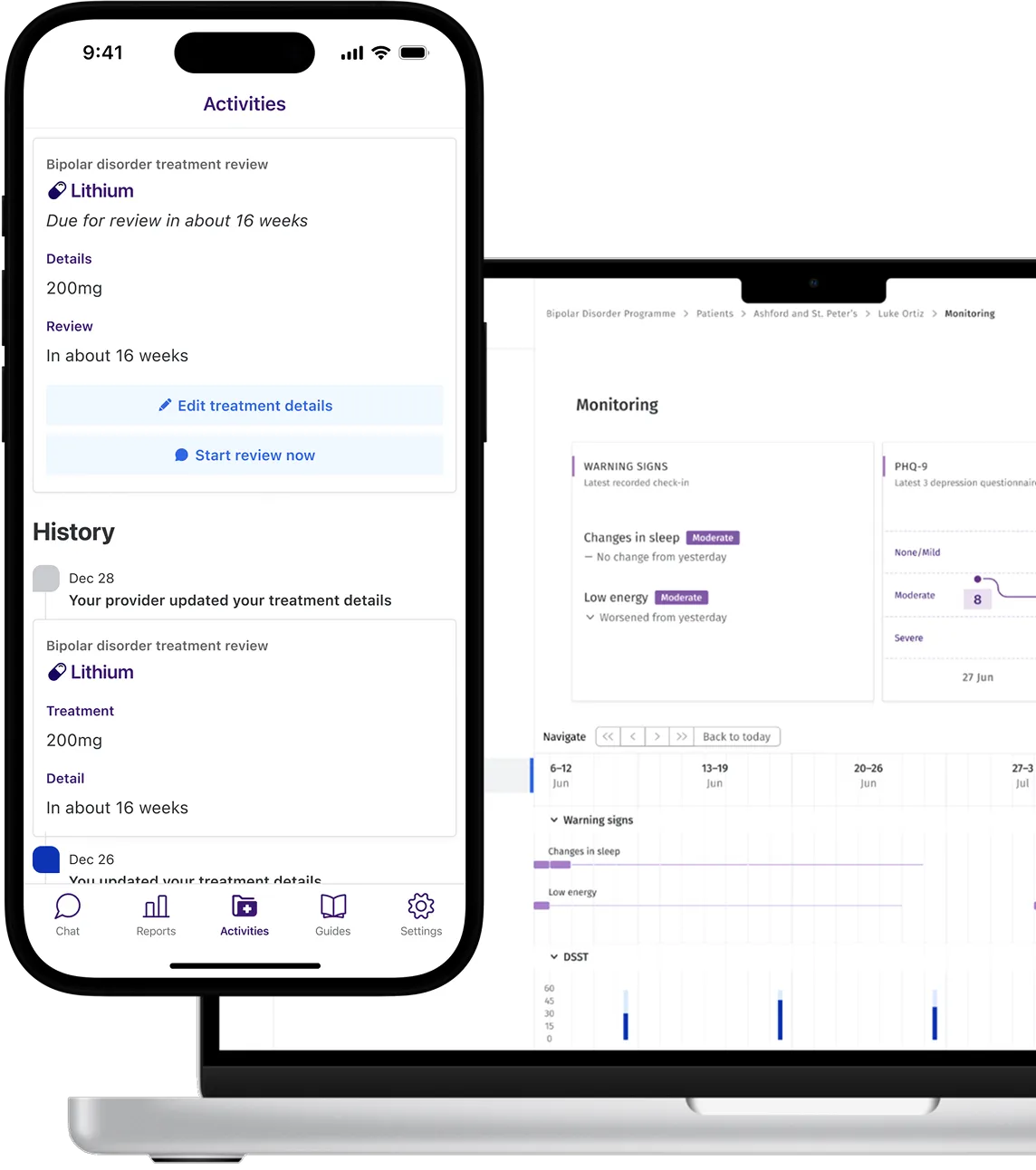
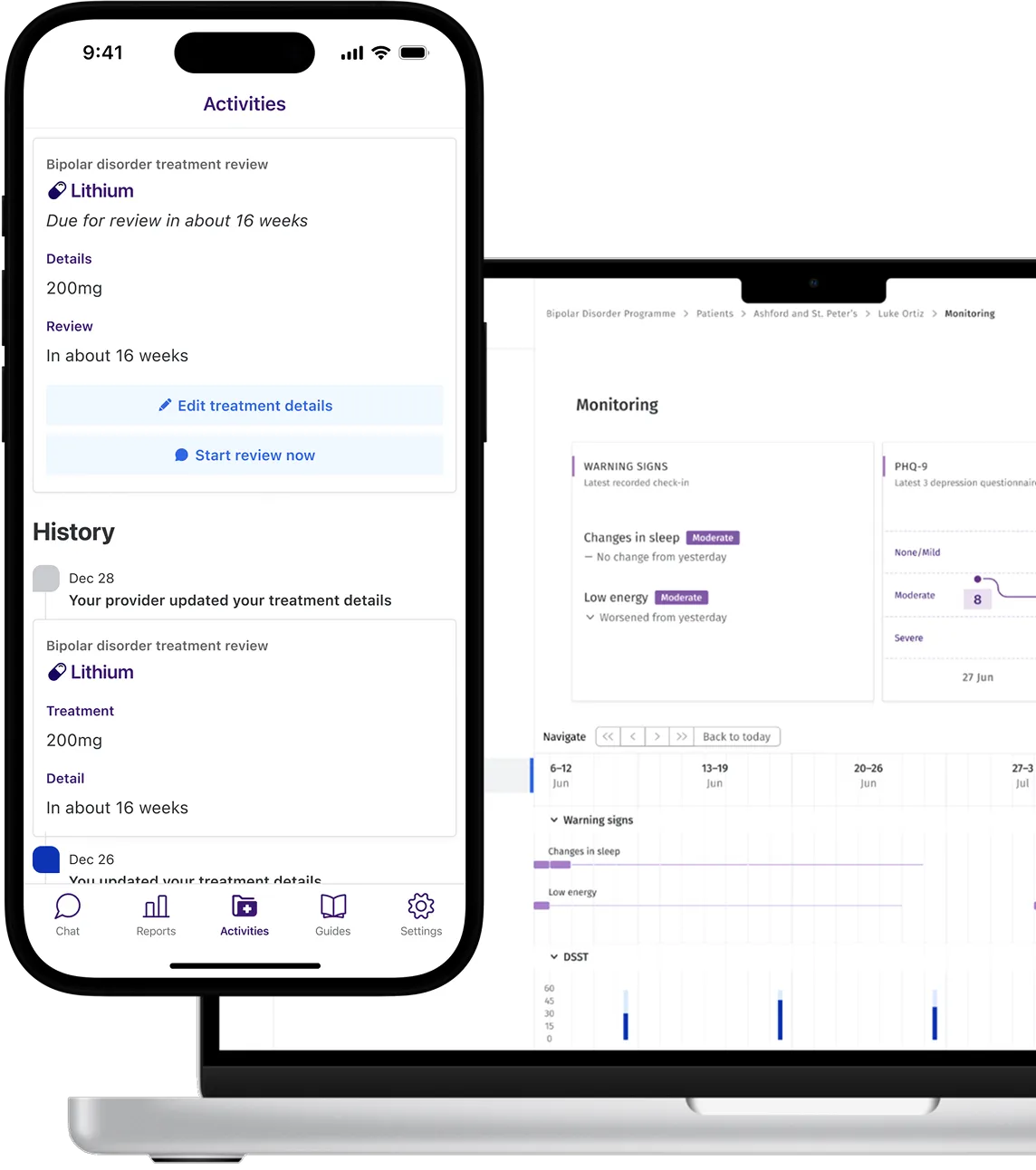
We presented people with lived experience of depression and bipolar disorder with a summary of Fora Health and proposed research to understand if this was clear and resonated with these user groups. Participants felt the summary was clear and that the service offered significant value in addressing their needs. However, they wanted more clarity about how the service related to in-person care and desired less clinical terms than adherence.
We asked participants about what factors to measure in a study evaluating the effectiveness and feasibility of a service like Fora Health. Participants associated effectiveness with improvements in one’s self-reported mood and symptom behaviours, like sleep and social interactions, and productivity. Effectiveness was also associated with improving the quality of interactions with providers. They felt these should be measured regularly using quantitative and qualitative approaches to capture nuanced changes in these domains. In terms of feasibility, participants noted that the service needs to be accessible and easy to use for patients and that there needs to be uptake of the service by healthcare providers and integration with healthcare systems. Participants also emphasised that secure and transparent data management is necessary for patients to trust and use the service.
We asked participants about which patients to include in the proposed study. While patients supported the inclusion criteria, they were concerned about excluding any patient in a manic or depressive episode, noting that it is important to research if Fora Health can support people in less severe episodes. While they understood the risk of including these participants, they wanted to ensure the exclusion criteria was not unnecessarily restrictive.
Finally, we got feedback on strategies to involve bipolar and depressive patients in planning and execution of the study. Participants were enthusiastic about having their voice heard in the design of the study and service, but first wanted to test and experience the service first hand. They emphasised the need to include diverse perspectives of not only patients, but also carers and healthcare providers. Participants also suggested making findings of the study accessible to wider audiences through collaborations with local community and healthcare organisations.